The research we conduct at Niagara Health has a profound impact on the health and well-being of our patients and communities, and contributes to better understanding some of the most significant healthcare challenges of our time and have the potential to benefit patients in Niagara and across Canada.
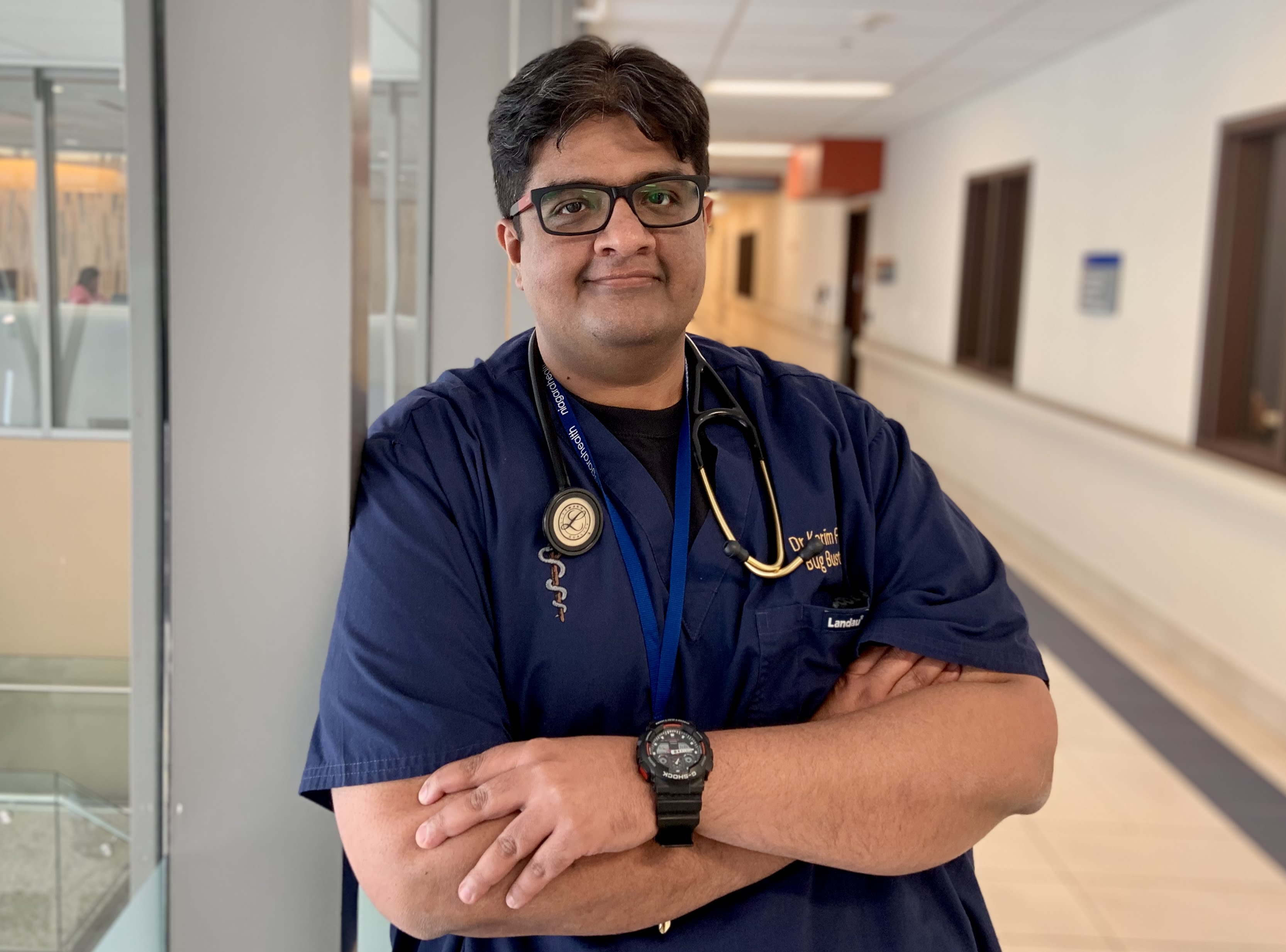
Dr. Karim Ali, Niagara Health’s Medical Director of Infection Prevention and Director, Division of Infectious Disease, is a co-author on an international study that found medical or surgical masks and N95 respirators work equally well when preventing the transmission of COVID-19 in healthcare workers.
Dr. Karim Ali knows that wearing a mask can help prevent the transmission of COVID-19.
As a co-author of a new study comparing medical masks and N95 respirators, Niagara Health’s Medical Director of Infection Prevention also knows that one isn’t better than the other.
Both medical masks and N95 respirators were found to work equally well against transmitting the respiratory virus.
“Masking is about filtering,” says Dr. Ali, also Director, Division of Infectious Disease. “Yes, N95 masks filter better but does that equate to a reduction in transmission of infection? It doesn’t.”
The findings were published last month in the Annals of Internal Medicine. The study, led by Dr. Mark Loeb at McMaster University, looked specifically at medical masks versus N95 respirators in preventing COVID-19 among healthcare workers and asked whether medical masks were “non-inferior” to N95 respirators.
“When healthcare workers are providing routine care to patients with a suspected case of COVID-19, they were non-inferior,” Dr. Ali says.
The study tracked 1,009 frontline healthcare workers in 29 acute care and long-term care facilities in Canada, Israel, Pakistan and Egypt between May 2020 and March 2022. Participants were randomly assigned one of the mask types and were able to opt out of the study at any time.
Niagara Health was an ideal candidate to participate in the study approved by research and ethics boards at all participating institutions because it experienced a high number of COVID-19 patients relative to other community hospitals, Dr. Ali explains.
“It made sense for us to be part of this,” he says. “It’s critical to note this was not to determine if masks work. This important study compares two types of masks.”
The research was inspired by debate early in the pandemic over which masks provided the best protection. Dr. Ali notes that many of the directives coming from public health organizations were confusing with some favouring N95 respirators over medical masks and later changing recommendations.
Meanwhile, some countries and regions had difficulty procuring N95 masks because of supply chain issues.
“When COVID-19 started, there was so much debate that continues today and so much polarization about infection transmission. People wondered, ‘If we’re not putting on N95 masks, are we doing a disservice to colleagues and loved ones?’” Dr. Ali recalls. “There was a lot of observational and feeling-based data but it does not stand up to scientific mettle.”
The study offers guidance for implementing COVID-19 masking policies and takes the emotion out of the process, he adds. It can also serve as a catalyst for future studies comparing masks in the context of influenza and respiratory syncytial virus (RSV).
“This is for public health and the Ministry of Health and Long-Term Care to look at critically,” Dr. Ali says. “At Niagara Health, medical masks must be worn when providing care and staff can upgrade personal protective equipment to N95 masks based on point of care risk assessment.”

