
Overcoming is a series of stories about our patients and their remarkable healthcare journeys.

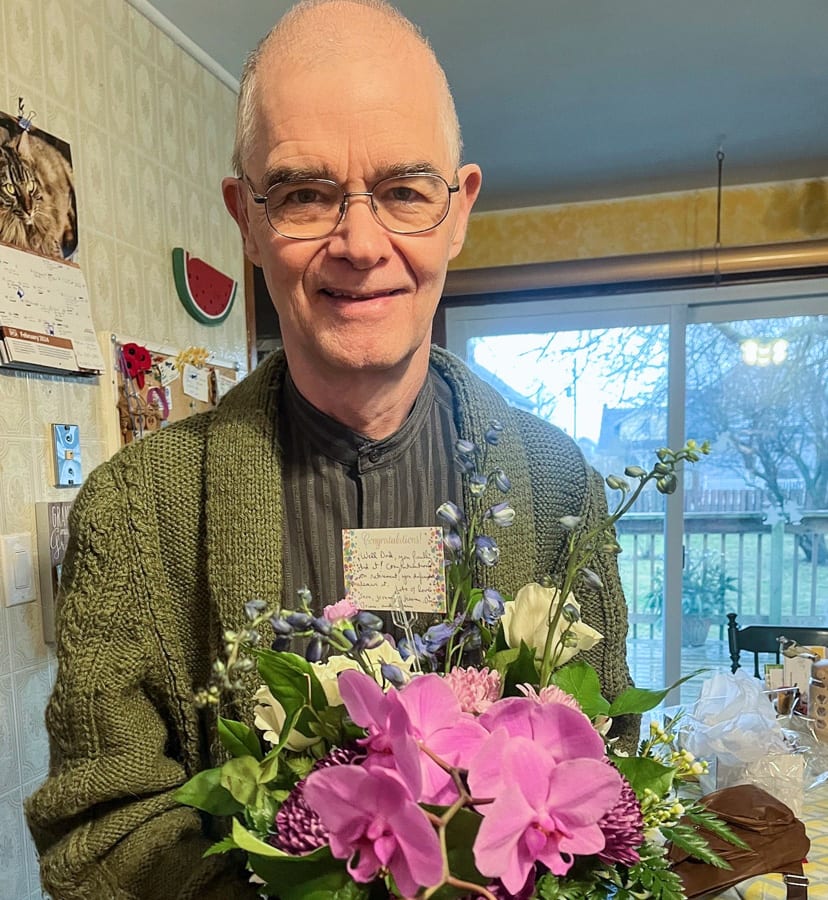
Rev. Bob Bond, seen here before retiring as Niagara Health chaplain, has been overcoming sepsis for nearly the past year.
When Rev. Bob Bond served as chaplain for Niagara Health, he saw the patients who called on him for spiritual care at a singular point in their healthcare journeys.
He would learn what brought them to the hospital but their lives after discharge remained unknown.
“I didn’t see from other people how their recovery goes on and on and on,” Rev. Bob said.
After decades working in healthcare, Rev. Bob is learning how long it can take to return to normal after time in the hospital for serious illness. He doesn’t have a definitive answer yet because his healthcare journey, which started nearly a year ago when he was diagnosed with sepsis, continues.
“This has been eye-opening,” he said. “I’m in the midst of on and on and on.”
The warning signs
It was Sept. 28, 2023 when Rev. Bob wrapped up his morning working at the Welland Hospital to head to a meeting in Niagara-on-the-Lake.
He wasn’t feeling well although he couldn’t pinpoint anything specific. At lunch before the meeting, his appetite was anemic. He had to concentrate more than usual to follow the conversation at the table. As the event progressed, a colleague told him he didn’t look well.
Heeding those cues, Rev. Bob headed home.
“It was a long walk to my car. I was light-headed. I let my wife know I was coming home,” he said. “In hindsight, I should have let her come get me.”
Once home, his wife, Lynn, suggested he go to the hospital. Rev. Bob figured rest would help. For months, stress had plagued him, impacting his ability to sleep more than 3.5 hours a night.
He woke up later that night and Lynn called 9-1-1. His blood pressure had plummeted to 50 over 30, which can be life-threatening if untreated.
“(Paramedics) were amazed I was talking to them. They worked like beavers and called another team to get me to the Welland Hospital,” Rev. Bob recalled.
Sepsis is a serious condition that happens when the immune system has an extreme reaction to an infection. It can lead to septic shock, including organ failure, and death if not recognized and treated early.
An immune system in overdrive
At the hospital, he was diagnosed with sepsis and admitted to the intensive care unit (ICU) before being transferred to the cardiac catheterization lab in Hamilton. That was the last thing he remembered about being in hospital there. He was admitted to the ICU in Hamilton and into the care intensivist Dr. Alison Fox-Robichaud, who is also the scientific director of Sepsis Canada and recognized globally for her sepsis leadership.
Sepsis is a serious condition that happens when the immune system has an extreme reaction to an infection. It can lead to septic shock, including organ failure, and death if not recognized and treated early. According to Statistics Canada, one in 18 deaths in Canada involves sepsis, while globally, the World Health Organization says sepsis accounts for one-fifth of all deaths.
It can develop from something as simple as a hangnail or from more severe illness, such as pneumonia. Those most vulnerable are older adults, children, immunocompromised and pregnant people.
Common signs of sepsis include fever, rapid breathing and heart rate. Other indicators include confusion or decreased level of consciousness, explained Dr. Jennifer Robert, Niagara Health’s Chief of Primary Care.
“It’s an infection any of us could get that progresses,” Dr. Robert said.
“The body knows what it’s doing in a crisis”
Family physicians can help determine the severity of an illness, including sepsis, by checking vital signs, she noted. But anyone with a suspected case needs to go to their nearest Emergency Department where bloodwork can be done to determine what’s happening.
“That’s where treatment is initiated, and it’s initiating that treatment as quickly as possible,” Dr. Robert said.
Rev. Bob was otherwise healthy when he developed sepsis. He pointed to the stress he felt, leaving him with little “oomph” to fend off the illness.
He was so sick by the time he got to Hamilton, Dr. Fox-Robichauld told Lynn he had 50-50 odds of making it through the night. He was intubated and on constant dialysis. Rev. Bob learned afterward he had “23 lines going into me, which is mind-boggling.” He also suffered a minor stroke and had to overcome pneumonia during his 10-day stay in the Hamilton ICU.
He was transferred back to the Welland ICU at that point, where he stayed for two weeks before spending nine more weeks on a medical floor, then moving to complex continuing care. By the time of discharge, he counted 104 days in hospital.
“I know from working in healthcare that staff are profoundly stressed but in the face of that, I received really fine care from a long list of physicians, nurses, nurse practitioners, respiratory therapists, physiotherapists, occupational therapists, speech language pathologists, dietitians, spiritual care and cleaning staff,” Rev. Bob said. “I can’t make a list long enough.”
At home, Rev. Bob continued his physiotherapy and needed diligent wound care for his toes, which became casualties of his sepsis by developing necrosis.
 “The body knows what it’s doing in a crisis,” he said. “Its focus is to protect the organs, and it says, ‘OK, the extremities, we can do without.’ When Lynn first saw my legs, from about halfway down from my knees to my toes, it was all black.”
“The body knows what it’s doing in a crisis,” he said. “Its focus is to protect the organs, and it says, ‘OK, the extremities, we can do without.’ When Lynn first saw my legs, from about halfway down from my knees to my toes, it was all black.”
Journey to recovery
Within six weeks of returning home, Rev. Bob was walking again. He connected with The Mayer Institute, a foot wound care centre in Hamilton, to treat the dead tissue his sepsis left behind. He started driving and fulfilling his retirement promise to Lynn to start doing all the jobs that had been downloaded to her, “starting with doing the dishes again.”
With an eye to healing, Rev. Bob retired from his spiritual care duties at Niagara Health. He stayed off his feet as much as possible while still trying to build his strength and relying on Lynn “who hasn’t missed a thing” as his caregiver.
Setback came in late July when his blood pressure began falling again and he returned to the Welland Emergency Department.
“We panicked and said, ‘Oh my gosh, this is how the sepsis started,” Rev. Bob said.
He was admitted to the Welland Hospital for two and half weeks for treatment of a bone infection in his toe.
“The battle goes on but from 11 months ago, it’s down to just a toe. So we’re getting there,” he said from his hospital bed. “It doesn’t happen overnight.”
Patients can return to their normal lives after sepsis, Dr. Robert noted, but prompt treatment is key.
So is prevention, she added. Fend off illness by ensuring vaccinations are up to date, washing hands and practising good personal hygiene. Even safe food handling can help. When infections happen, treat them early to prevent them from becoming something worse.
“If you’re feeling unwell in any type of way, seek the appropriate medical attention, whether it’s your family physician or, if it’s more serious, coming to the hospital, rather than getting to the point where your life may be at risk, because this is treatable as long as it’s done in a timely manner,” Dr. Robert said.
Rev. Bob remains hopeful the end of his sepsis healthcare journey is in sight. Once his toe heals, he’ll focus on building his strength so he can enjoy retirement to the fullest. That means finding his next calling and playing with his grandchildren, he said. Getting back to household duties and relieving Lynn is also “high on the list,” as is paying attention to what his body is telling him at any given moment.
“It’s worth letting the world know what this is,” he said. “My only symptom was light-headedness. If a person is experiencing dizziness and their blood pressure is falling, don’t ignore that.”
Photo: (Above Right) Rev. Bob Bond after he was released from the hospital last winter. Rev. Bob spent 104 days in hospital in Welland and Hamilton at the time, overcoming sepsis.

