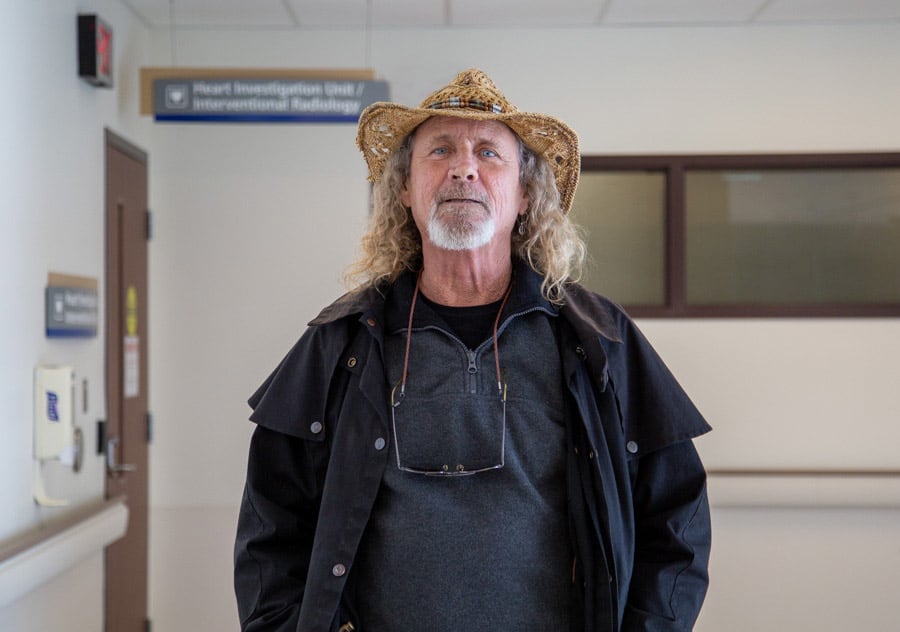
Niagara Falls resident Perry Wintle was the first patient to undergo the shockwave procedure at Niagara Health when the technology arrived at the Marotta Family Hospital in January.
Perry Wintle’s cardiovascular health journey is on track thanks to a new, life-saving procedure now available at Niagara Health.
Recently, Wintle became the first patient to undergo intravascular lithotripsy, a minimally invasive therapy that uses ultrasound shockwaves to break up hardened calcium deposits, making it easier to treat blocked arteries closer to home and prevent serious cardiac events.
“It’s a great thing for St. Catharines to have – and Niagara region,” Wintle said. “It’s long overdue, I imagine.”
When the Niagara Falls resident arrived at the Heart Investigation Unit at the Marotta Family Hospital in late January for an angioplasty to insert stents, neither he nor Dr. Sanjit Jolly, the interventional cardiologist performing the procedure, expected to find his arteries 80 per cent blocked with calcium.
Thanks to the newly acquired Shockwave Medical equipment, however, Dr. Jolly quickly cleared the blockage and continued the procedure. Before this technology, he would have been forced to halt the angioplasty – done to improve blood flow – and send Wintle out of region for treatment. That would have delayed care for weeks, increasing the risk of a life-threatening cardiac event.
Not all blockages are caused by calcium. Patients with blockages comprised of lipid or fibrotic tissue typically don’t require intravascular lithotripsy.
“(Calcium deposits) are like rocks. You can’t expand the (angioplasty) balloon or insert a stent,” Dr. Jolly said. “For people with calcified disease, this is an important treatment option.”
How the Shockwave procedure works
A fluid-filled balloon catheter is placed against the calcified blockage in the artery and releases 120 acoustic pulses in intervals of 10 with short breaks between. This process breaks up the calcium without harming blood vessels.
The therapy takes about five minutes, followed by 45 minutes to an hour for the angioplasty.
Before the arrival of the technology, Dr. Jolly, who also practises at Hamilton Health Sciences, encountered at least one patient a week with calcified plaque who needed to be referred elsewhere. Patients often waited up to a month before they could undergo the full procedure, usually in Hamilton.
Calcified blockages are difficult to detect until the angioplasty begins, explained Matthew Baronaitis, Clinical Manager of Cardiology. While a cardiac CT scan can reveal calcium buildup beforehand, scheduling those scans for every patient isn’t feasible.
Additionally, CT scans expose patients to significant radiation – equivalent to “a few hundred X-rays” – on top of radiation from the angioplasty itself.
Previously, patients at the Marotta Family Hospital would be sedated, injected with dye to highlight arteries and blockages, and only then discover once the angioplasty catheter was inserted that the blockage was due to calcium, forcing doctors to stop the procedure.
“A patient, already anxious about the angiogram, could have been mid-procedure, only to find out there was nothing we could do to fix the blockages. They would then have to be recovered and re-booked in Hamilton to have the procedure done again,” Baronaitis said. “I believe that adds additional stress to the patient.”

Dr. Sanjit Jolly
The new technology not only eliminates that uncertainty, it also streamlines patient care in the Heart Investigation Unit, allowing more patients to receive timely treatment, he added.
A life-saving intervention
Time was of the essence for Wintle, who only discovered his blockages when he developed jaundice and was diagnosed with pancreatic cancer last October.
Wintle recalled the radiologist reviewing his diagnostic imaging and asking if he had a stent in his chest. When Wintle said no, the physician realized it was a blockage, and an angioplasty was scheduled.
“If it had gone unnoticed, it could have killed me,” Wintle said. “There were so many opportunities for it to be overlooked.”

The Niagara Health team that performed the first shockwave procedure. Rachel Moxham (dark grey scrubs), Senior Field Clinical Specialist with Shockwave Medical, is a former Medical Radiation Technologist with Niagara Health.
Wintle’s daughter Cassandra, a nurse in the Marotta Family Hospital Intensive Care Unit, knows the impact of receiving timely care.
“Patients suffer when they don’t have access to treatments,” Cassandra said. “When you’re walking around with an 80-per cent blockage, your days may be limited, and you don’t know what’s going to happen.”
Wintle’s care team advised him to have surgery for his tumour first, then undergo the angioplasty. That timeline allowed for what he calls “the alignment of the stars.” By the time he was ready for the procedure, the Shockwave Medical technology had arrived in Niagara.
“I’m a lucky man – a very lucky man. They caught my cancer and my heart problems,” said Wintle, who is now undergoing chemotherapy at the Walker Family Cancer Centre.
Other than being a little groggy after the shockwave treatment and angioplasty, he said he felt like himself again.
“It’s fantastic to be able to have the full treatment and walk out the same day,” Wintle said. “It’s day surgery at its finest.”

