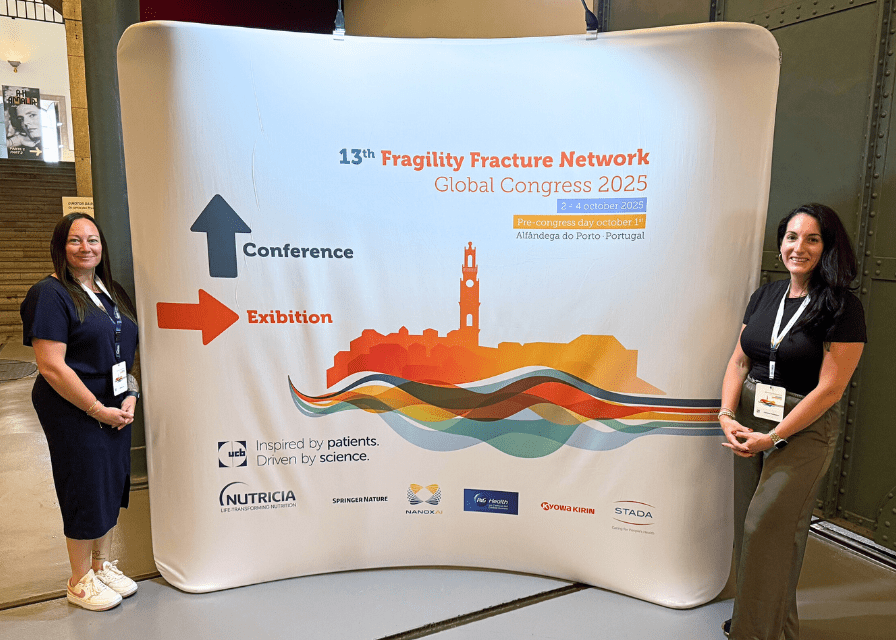
Program Manager Stefanie Irish and Nurse Practitioner Christina Huntington represented Niagara Health at the Fragility Fracture Network meeting in Portugal, sharing the organization's interprofessional orthogeriatrics model with clinicians from around the world.
A Niagara Health program aimed at improving care for older adults with hip fractures is attracting attention from clinicians around the world.
The orthogeriatric consultation service, launched last year and led by Nurse Practitioner Christina Huntington at the Niagara Falls Hospital, brings together an interprofessional team, recognizing the complexities of older adults and the value of co-ordinated care and assessments.
The team works collaboratively to reduce the number of times that patients and families share their story and strives to plan post-operative treatment and therapy. They also support early mobility and promote a safe recovery, such as early delirium identification and management.
The result is faster healing, shorter hospital stays and smoother transitions home.
“Patients love when they can see all of us at once,” Huntington says. “They don’t have to retell their story three times, and it means we’re all working toward the same goal in the same moment.”
Launched in March 2024, the service began with patients 85 and older recovering from hip fractures. As the model proved successful and team familiarity grew, it expanded to include patients 75 and older, with a goal to reach 70 and older by the end of 2025.
The team’s collaboration earned them Niagara Health’s Interprofessional Collaboration Award earlier this year in recognition of the program’s innovation in patient-centred care and its impact on outcomes.
“They [patients] don’t have to retell their story three times, and it means we’re all working toward the same goal in the same moment."
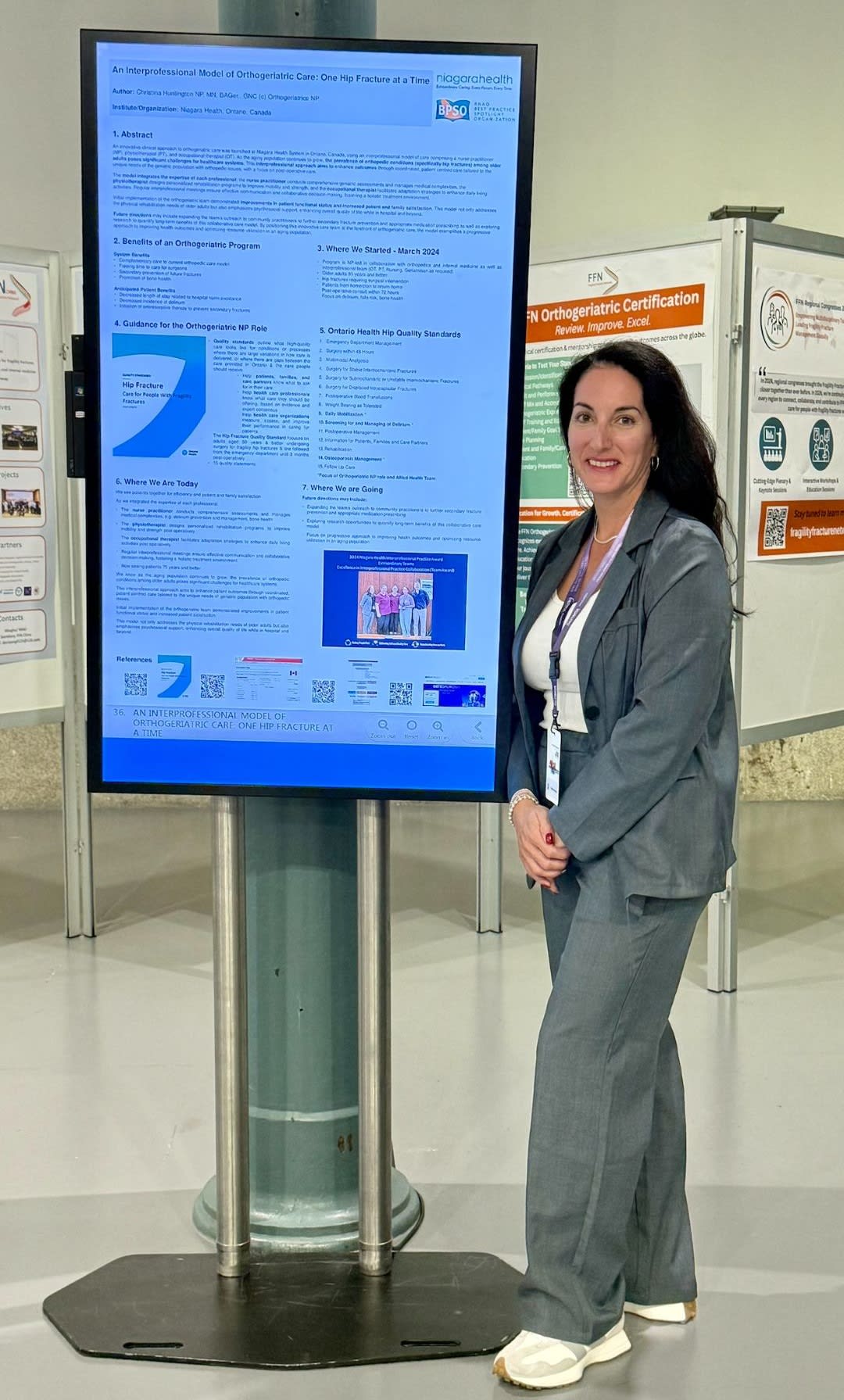
Christina Huntington showcased how Niagara Health's ortho-geriatric model is transforming hip fracture recovery through teamwork and person-centred care.
Taking Niagara Health to the world stage
Building on that success, Huntington presented the team’s work at the Canadian Gerontological Nursing Association (CGNA) conference in Winnipeg this spring before sharing it internationally at the Fragility Fracture Network (FFN) meeting in Portugal - a leading global forum focused exclusively on orthogeriatric care.
Program Manager Stefanie Irish joined Huntington at the FFN meeting to broaden Niagara Health’s expertise and strengthen ties with leaders advancing similar models worldwide.
“It was incredible to see how much global interest there is in orthogeriatrics,” Huntington says. “Standing in that room, surrounded by people from all over the world who care about the same work, really validated that our approach in Niagara is on the right path.”
Bringing lessons home
The global exchange inspired two new areas of focus that Huntington and the geriatrics team are already working to integrate:
- Secondary fracture prevention: introducing evidence-based medication earlier to help prevent additional fractures in the future.
- Protein and nutrition: involving dietitians earlier in recovery planning to help patients rebuild strength and reduce complications.
Huntington is collaborating with Benson Lam, Niagara Health’s geriatrics pharmacist, and Jennifer Mulligan, a clinical dietitian, to explore how these practices can be formally embedded across the program.
“These are simple, evidence-based changes that can help patients leave the hospital stronger and reduce the chance of readmission,” Huntington says.
The program’s success continues to be driven by interprofessional teamwork. With multiple disciplines in the same room, care becomes more efficient, co-ordinated and patient-centred.
“For example, If a patient feels dizzy or hesitant to stand, we can assess and make decisions together right there,” Huntington explains. “That kind of collaboration helps patients move safely and it helps staff feel supported, too.”
While the model continues to expand, its foundation remains the same: treating every patient as a person first.
“When we take a few minutes to learn about someone — what matters to them, what brings them joy -- that changes everything,” says Huntington. “That’s what person-centred care really means.”

