When Tammy Vande Wiel slipped and fell outside her apartment on a cold January morning, she had no idea how long the road to recovery would be. With a broken femur and wrist on her dominant side, even the simplest tasks such as bathing, eating and standing became difficult.
After surgery and several weeks in hospital, Vande Wiel’s care team introduced her to Donna Mantesso, Niagara Health at Home (NH@Home) Program Coordinator. Vande Wiel was a prime candidate for the program.
“I slipped on ice and fell outside of my apartment building going to work,” she says, recalling how something that seems small like a fall can have such a big impact on your life and mobility.
She credits being part of NH@Home and determination with her ongoing recovery.
“Patients simply do better at home,” says Mantesso. “Hospitalization can lead to higher risk of infections or delirium or deconditioning. Being surrounded by loved ones, familiar belongings, and pets at home creates a comforting environment where patients regain their routines and confidence more quickly.”
Launched in December 2024, NH@Home is part of a growing provincial effort under Ontario Health to reimagine how patients transition from hospital to home.
“The purpose is twofold. It’s to help reduce alternate level of care (ALC) patients in hospital by partnering with patients to deliver the essential supports that make successful home recovery possible,” says Lisa Hildebrand, Director of Access and Flow and the Regional Stroke Program at Niagara Health. “It also aligns with Ontario Health’s goal to modernize our healthcare system by putting a home-first philosophy into practice.”
That philosophy is helping people heal where they feel safest and most supported. It has already helped more than 430 patients heal at home since the program’s launch late last year.
Vande Wiel’s recovery began at Niagara Health’s St. Catharines and Fort Erie sites, where she spent almost two months recovering.
“On March 14, I finally came home,” Vande Wiel says as she references her phone’s calendar, where all appointment dates, consultations and details of her care journey are meticulously noted.
She says the next day, a nurse visited her home to assess her and by March 17, she had visits from Personal Support Workers (PSWs) in place.
“I had someone here every single day at the start of the program. The visits were less frequent as my recovery improved,” she says.
Through NH@Home, and in partnership with Bayshore, Vande Wiel received a coordinated care plan that included visits from nurses, PSWs, social workers and physiotherapists.
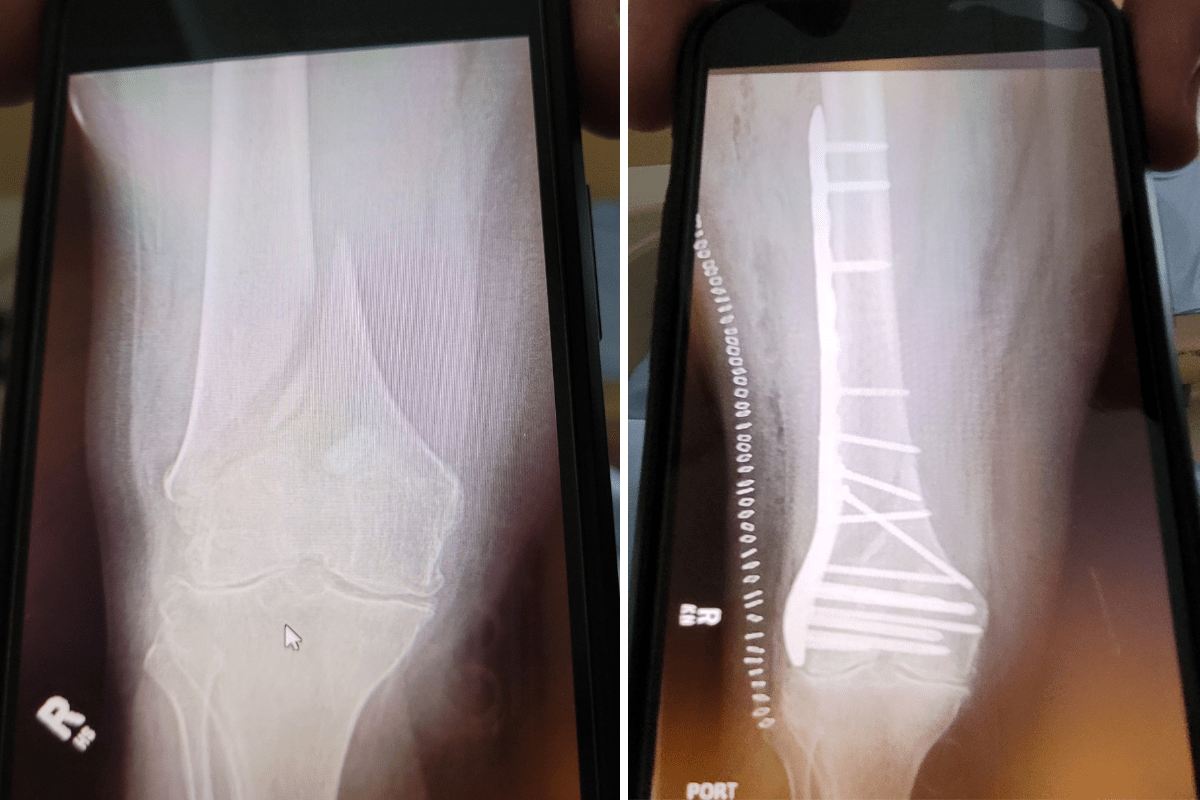
X-ray image of Tammy Vande Wiel’s femur fracture before, left, and after surgery, right.
“They really made a difference,” she says. “Some PSWs even went above and beyond with tasks that were difficult for me, like washing dishes.”
For Vande Wiel, regaining independence wasn’t just physical, it was emotional.
“When I was in the hospital, I was in bed most of the time,” she says. “At home, I forced myself to move. I’d make sure to get up for a drink, even when it was hard. Being in my own space motivated me.”
She says her physiotherapist guided her every step of the way, from simple leg lifts to walking hallways and climbing stairs.
“She didn’t just answer my questions; she took the time to explain everything to my son and my friend Michelle (McFarlane) as well,” Vande Wiel says.
Mantesso remembers working with Vande Wiel before her discharge.
“Initially, she was fearful about coping at home,” she says. “But once we walked through her care plan, she realized she wouldn’t be alone. I told her getting back into your daily routine around your family is therapy too. She really embraced that.”
The philosophy of NH@Home is simple: recovery is most effective in familiar surroundings that empower patients to restore their comfort, confidence and independence.
“Most people have pets or family they miss deeply while in hospital. Being home means they can recover surrounded by what and who they love. That’s incredibly powerful for healing,” Hildebrand says.

Tammy Vande Wiel sits upright with her knees bent, a simple movement she could not do a few months ago, left. Tammy Vande Wiel stirs a pot of homemade soup, a movement she is now able to do after months of physiotherapy rehabilitation and exercises, right.
Vande Wiel’s support network extended beyond healthcare providers. Her son Dylan helped around the house, while her life-long friend McFarlane visited regularly to provide even more support. Her parents also brought her a reclining chair so she can rest comfortably.
Vande Wiel’s son says the difference in his mother was immediate when she left hospital.
“She was in pain, but less frustrated,” he says. “Being home made her more relaxed. She could read, watch TV and have visitors. It was easier for her to focus on getting better.”
McFarlane agrees. “Tammy’s one of the most determined people I know. She doesn’t like relying on others. She wanted to be herself again and she is working so hard for that.”
“The program gives you the tools,” Tammy Vande Wiel says. “But you have to do the work. You have to want to get better.
“When I started walking the hallways and climbing the stairs with my physiotherapist, that’s when I knew I’d get through this,” she says. “Now, I can walk around without a cane or walker outside of my home.”
Each NH@Home patient is referred through their care team and is assessed for eligibility.
“Each patient case is different,” Mantesso explains. “I consult with patients and their families to review their requirements, what the program has to offer and answer any questions.”
After consultation, a tailored care plan is created and can include any combination of the supports needed, including PSWs, nursing, physiotherapy, occupational therapy, speech language pathology, social workers or registered dieticians.
Currently, the NH@Home program offers two care “bundles”: an eight-week and a 16-week option, depending on the patient’s needs. Care teams monitor progress weekly and adjust support as needed, working hand in hand with enrolled patients and their families.
The patient’s living space is also assessed and equipment is provided to help with home recovery. For Vande Wiel this included a wheelchair, a walker with an additional arm piece, shower bench and elevated toilet seat for accessibility.
“The goal is to restore individuals to their highest possible level of independence," Mantesso says.
Hildebrand says the program results have been incredible.
“We’ve exceeded our targets and have seen people recover faster and happier at home. That’s the power of this program,” she says.
For Vande Wiel, being home wasn’t just about comfort, it was about control.
“At home, I could set my own schedule,” she says. “I could eat and sleep when I wanted. I wasn’t waiting for nurses or sharing a room. I could just focus on getting better.”
Now, she’s back to walking without a cane or walker, attending physiotherapy, planning her return to work and very recently started driving again.
“I’m getting there,” Vande Wiel says proudly. “I just need to make sure my wrist is strong enough to type for work again. I’m not rushing, it’s about getting back to being me.”

